Y Gell Cyngor Technegol: crynodeb o'r cyngor 6 Awst 2021
Crynodeb o'r cyngor COVID-19 a ddarparwyd i Weinidogion Cymru ar 6 Awst 2021.
Efallai na fydd y ffeil hon yn gyfan gwbl hygyrch.
Ar y dudalen hon
Top line summary
Overall, case numbers have decreased across the majority of Welsh Local Authorities, with case incidence at a national level decreasing by 14% in the most recent week to 133.4 cases per 100,000 population. This sharp downward trend has also been seen in other areas of the UK where the third wave of the pandemic was more developed than Wales. There remains considerable uncertainty and further analysis to understand the cause and implications of this trend is required.
The most recent variant technical briefings and assessments from Public Health England indicate that B.621 is still considered a Variant Under Investigation, but is not assessed to be a significant risk at present as current evidence shows that it is outcompeted by Delta.
Observed levels of COVID-19 admissions to hospital, deaths and hospital bed occupancy are roughly at the levels estimated by the June 2021 most likely scenario (MLS). COVID-19 admissions to ICU were rising faster than the June 2021 MLS, but is now decreasing and are relatively low.
CoMix data shows that mean reported contacts (in the UK) do not appear to have increased since the easing of restrictions on 19 July 2021. Overall, contacts amongst adults remain stable, whereas contacts for children have decreased sharply now that schools have closed.
In a study investigating public use of lateral flow test (LFT) or polymerase chain reaction (PCR) test, it was found that a significant percentage of the population use LFT tests when symptomatic. This was attributed to the easy accessibility, short turnaround time and lack of requirement to formally register the test (and subsequently self-isolate on a positive test). Communications should emphasise the superiority of, and need for, PCR tests if symptomatic.
Implications from a study modelling the conditions that may increase the risk of the emergence and establishment of a vaccine-resistant variant of COVID-19 suggest that policymakers and individuals should consider maintaining non-pharmaceutical interventions and transmission-reducing behaviours throughout the entire vaccination period.
A multi-centre cohort study (pre-print; not yet peer-reviewed) suggests that mRNA vaccines are highly effective at preventing symptomatic and severe COVID-19 associated with infection with the Delta variant. Vaccination is associated with faster decline in viral RNA load and a robust serological response. It concludes that vaccination remains a key strategy for control of COVID-19 pandemic.
Findings from the Zoe COVID symptom study show that whilst COVID-19 in children is usually short, with low symptom burden, some experience prolonged illness. However findings suggest that symptom burden in these children did not increase with time, and most recovered by day 56. It is important to note that this data is reported by parents and depended upon an adult with access and capacity to participate.
An update from the Advisory Committee on Immunization Practices after reports of myocarditis among vaccine recipients, concluded that the benefits of mRNA COVID-19 vaccine outweigh the risks, including in adolescents and young adults, although there was recognition the balance of benefits and risks varied by age and sex. Outcomes of myocarditis cases will continue to be monitored and it was recommended that providers and the public should be informed about these cases to inform their own risk assessment, particularly for males aged 12-29 years.
Data from a qualitative study of public attitudes towards COVID-19 vaccination in children (pre-print; not yet peer-reviewed) identified six themes: (1) Uncertainty over whether children can catch, transmit or be severely harmed by COVID-19; (2) Lower risk tolerance for unknown longer-term effects of the vaccine in children; (3) Association of the vaccine program with government’s handling of the pandemic; (4) Local social norms as a driver of hesitancy; (5) Vaccinating children as a way to protect vulnerable adults; (6) Children’s vaccination as parental choice.
Long-term negative outcomes in healthcare workers from exposure to potentially morally injurious experiences and consequent impacts for patients and the organisations they work in are not inevitable. Health care workers, their colleagues, and leaders can use strategies to improve outcomes both during and after potential morally injurious situations, to support recovery and potentially even gain insights and new ways of working. See TAG report for more information.
A recent systematic scoping review on Long COVID highlights that fatigue, breathlessness, arthralgia, sleep difficulties, and chest pain are predominant symptoms; there is a risk of long-term sequela and that lack of a universally accepted definition has impaired its proper recognition and management.
TAG modelling of the impact of TTP on COVID-19 transmission in Wales (soon to be published) notes that the removal of self-isolation restrictions on 7 August 2021 for contacts who are under 18 or fully (double) vaccinated is estimated to increase Rt by 0.3 (at an Rt of 1.4 as estimated by SPI-M on 15 July) compared to the original self-isolation rules where all contacts are required to self-isolate.
TAG modelling of COVID-19 population immunity estimates in Wales estimates that close to 90% of the Welsh population, spread evenly across Wales, must be immune to COVID-19 before population immunity effects could be observed.
Advice from the Technical Advisory Group and the Chief Scientific Advisor for Health (30 July 2021) to inform the most recent 21-day review is available here (soon to be published).
Wales Sit-Rep
Read the latest COVID-19 Situational Report, containing the most recent data on epidemiological surveillance, NHS status, education and children, international travel, mobility, vaccination and immunity and forward projections.
Overall, case numbers have decreased across the majority of Welsh Local Authorities, with case incidence at a national level decreasing by 14% in the most recent week to 133.4 cases per 100,000 population. This sharp downward trend has also been seen in other areas of the UK where the third wave of the pandemic was more developed than Wales. Factors that might have a part to play in this reduction include population level behavioural changes, closing of schools, good weather, impact of vaccine rollout and more. There remains considerable uncertainty and further analysis to understand the cause and implications of this trend is required.
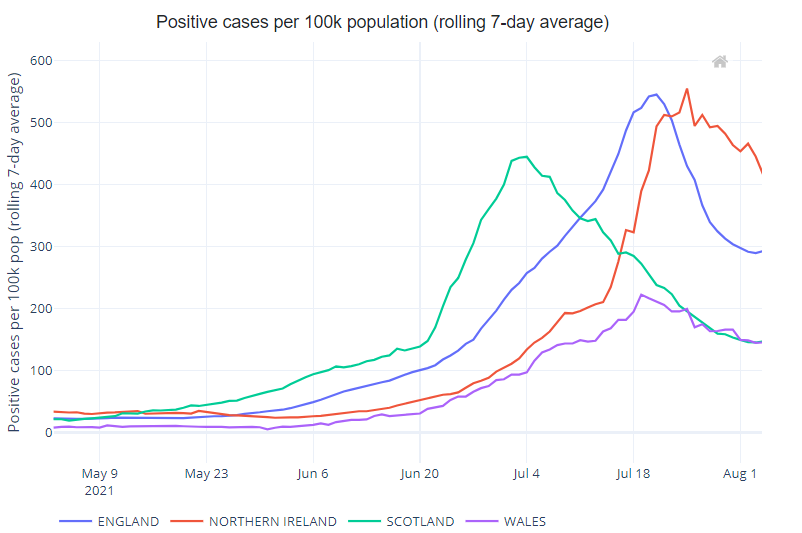
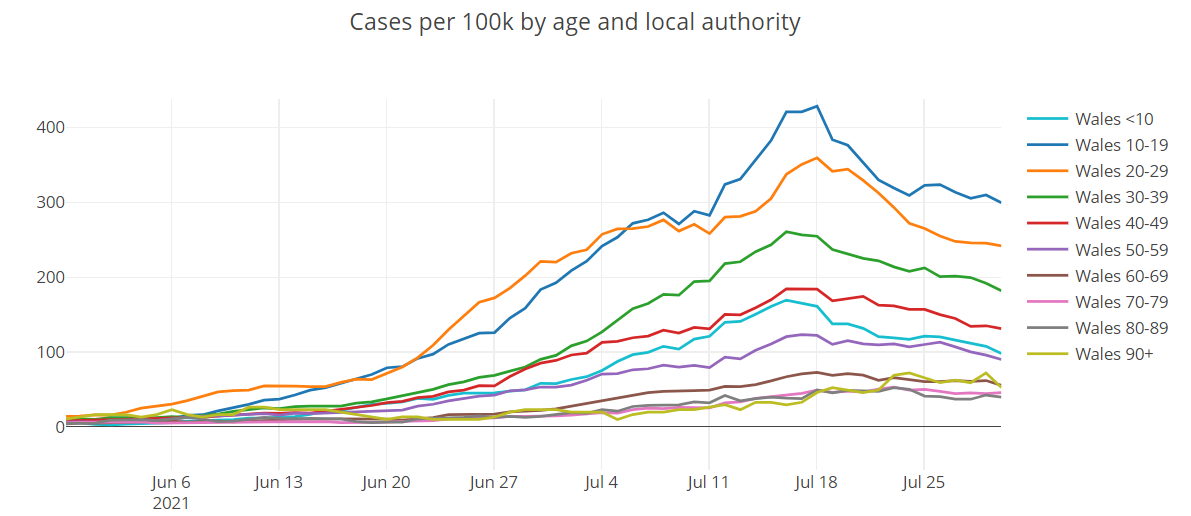
Case numbers have decreased in all age groups but continue to be highest in the 10-19 and 20-29 age groups, although the extent of the difference with other age groups varies by local authority.
The JBC consensus estimate of Reproduction number (Rt) for Wales is between 0.8 and 1.1 (as at 5 August 2021), with a daily growth rate of between –3% and +1% and a halving time of 29 days to flat. Note this is typically lagged by 2-3 weeks.
PHW’s national estimate of Rt, which is lagged by around 1 week, is an Rt of 0.85 for Wales and a national halving time of 65 days. When R is below 1.0, the pandemic is shrinking.
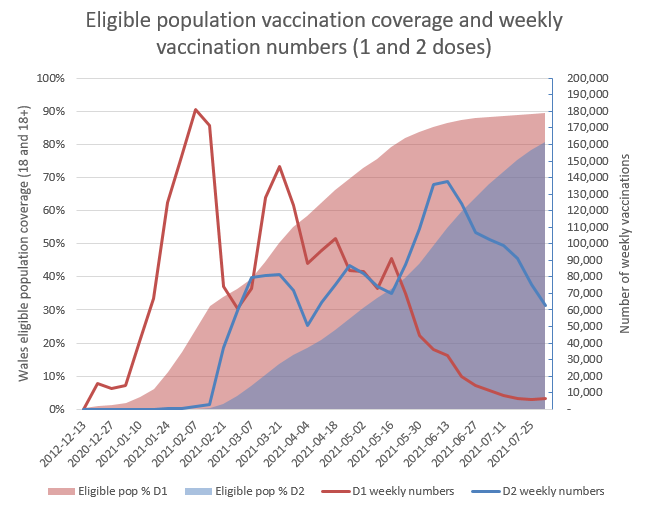
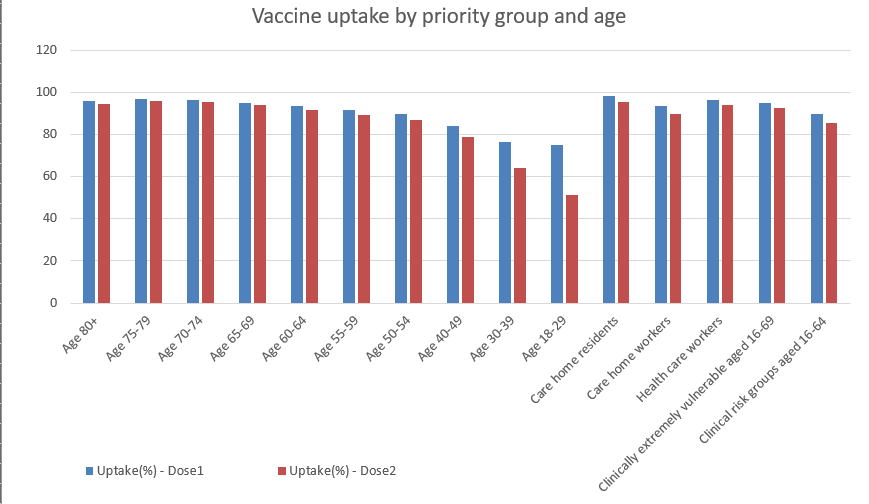
With 90% of the eligible Welsh population having received their first dose of the vaccine (excluding the recent JCVI recommendation to expand first doses to 16 and 17 year olds), focus has largely shifted to giving people their second dose, with first dose take up for the 18-29 and 30-39 age groups stabilising at around 75%. Welsh Government are now working with the NHS on the arrangements needed to offer the vaccination to all 16 and 17 year olds in line with the JCVI advice and this will be included once rollout begins.
Reasonable worst case and most likely scenarios versus actual figures
Key message: Confirmed COVID-19 cases increased throughout June and the first half of July, but decreased in the second half of July. Observed levels of COVID-19 admissions to hospital, deaths and hospital bed occupancy are roughly at the levels estimated by the June 2021 most likely scenario (MLS). COVID-19 admissions to ICU was rising faster than the June 2021, but is now decreasing and are relatively low.
The report below compares observed levels of COVID-19 indicators with the June 2021 reasonable worst case (RWC) scenario and most likely scenario (MLS) for the first time. These scenarios take account of the impact of the Delta variant.
In the charts below “RWC_Jun2021” is the June 2021 RWC scenario, “MLS_Jun2021” is the current (June 2021) most likely scenario, and “Actuals” represents the actual observed values for each indicator.
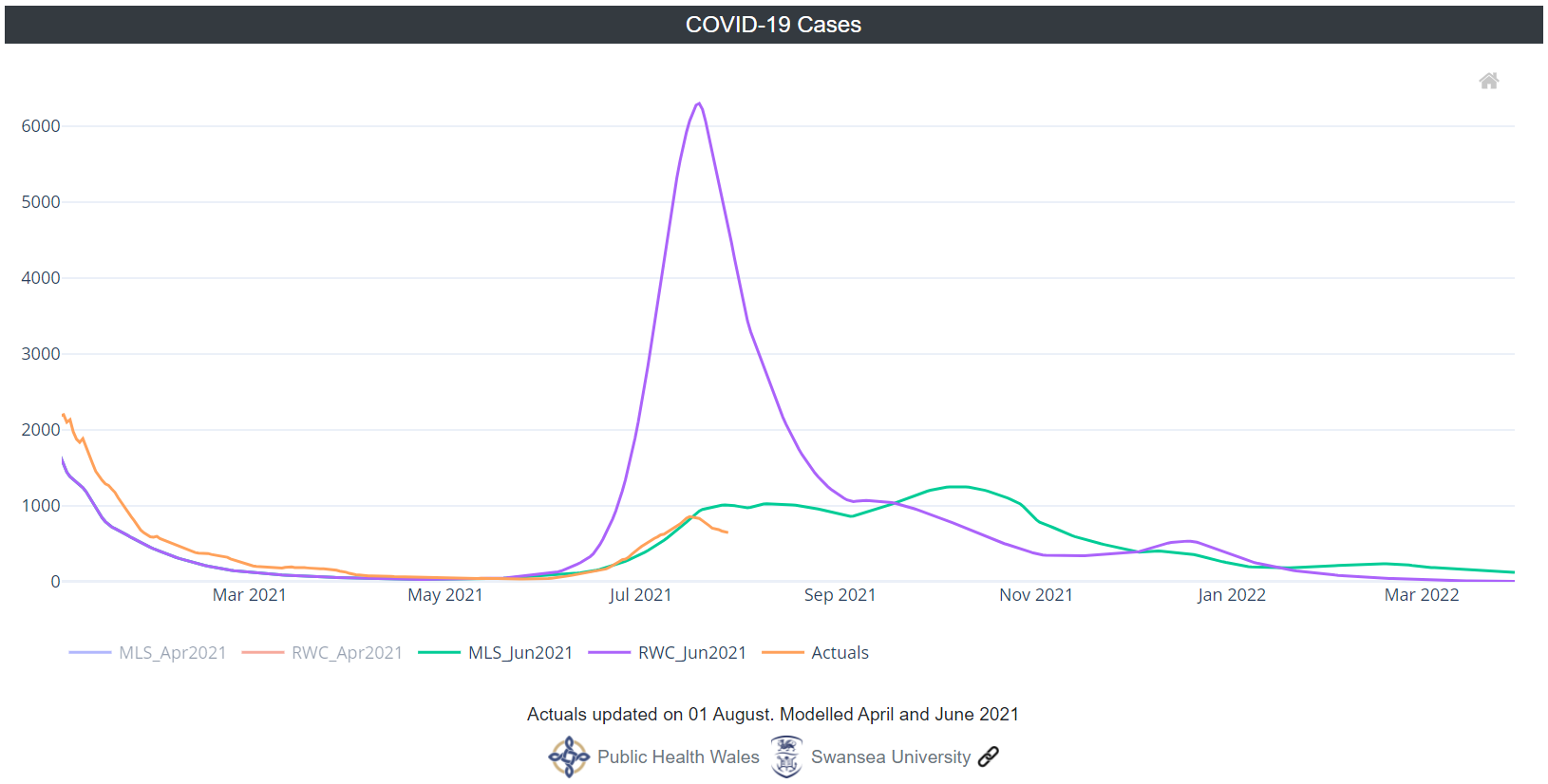
Confirmed COVID-19 cases were low and stable throughout April and May but started to rise in June 2021. They peaked on 16July 2021 and has been falling since. Through June and much of July confirmed COVID-19 cases followed the MLS very closely. On 30 July this indicator was below the MLS. Note that for the model scenarios, “Cases” refers to symptomatic cases only so may be an underestimate.

COVID-19 hospital admissions decreased slowly in May and June 2021 before starting to increase in July. They increased throughout July, staying just above the levels forecast by the MLS. On 30 July the 7-day average for COVID-19 hospital admissions was just above the MLS at 16 admissions per day.
In May and June 2021 COVID-19 ICU hospital admissions were very low and stable. They rose in early July, reached a peak on 19 July 2021 and then started to fall. On 30 July 2021 the 7-day average for COVID-19 ICU hospital admissions was just under 2 per day, which is between the MLS and RWC.
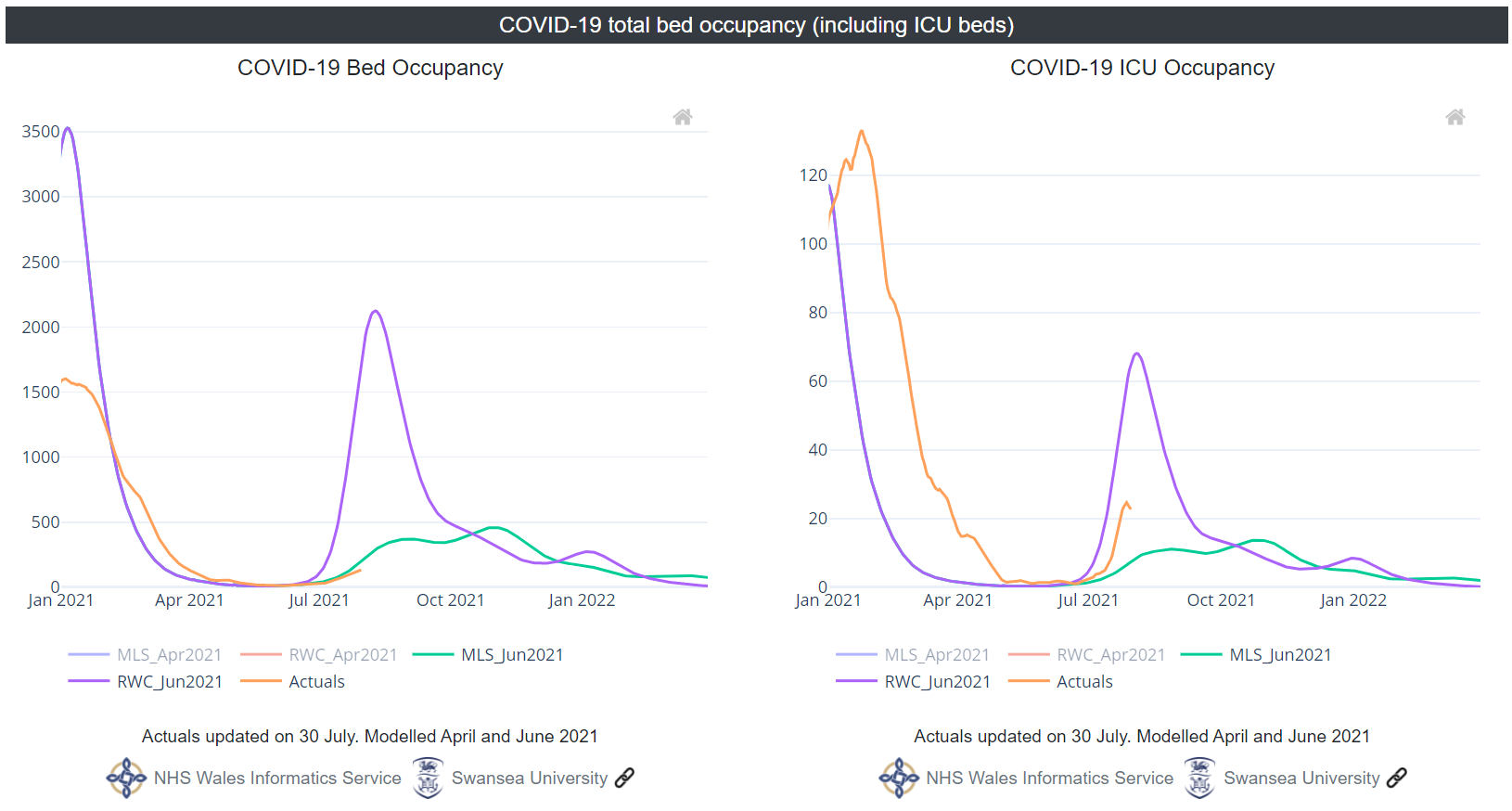
COVID-19 confirmed total bed occupancy (which includes ICU beds) was low and stable throughout May and June and started to rise in early July. As of 30 July 2021 the 7-day average for COVID-19 confirmed total bed occupancy was a little over 134 beds occupied by COVID-19 confirmed patients – just under the level forecast by the MLS.
Through most of May and June COVID-19 confirmed ICU occupancy was very low at between 1 and 2 per day. It began to rise in early July, about 10 days later than forecast by the RWC, and rose at a rate similar to the RWC. As of 30 July 2021 COVID-19 confirmed ICU occupancy was just under 23, which is between the MLS and RWC.
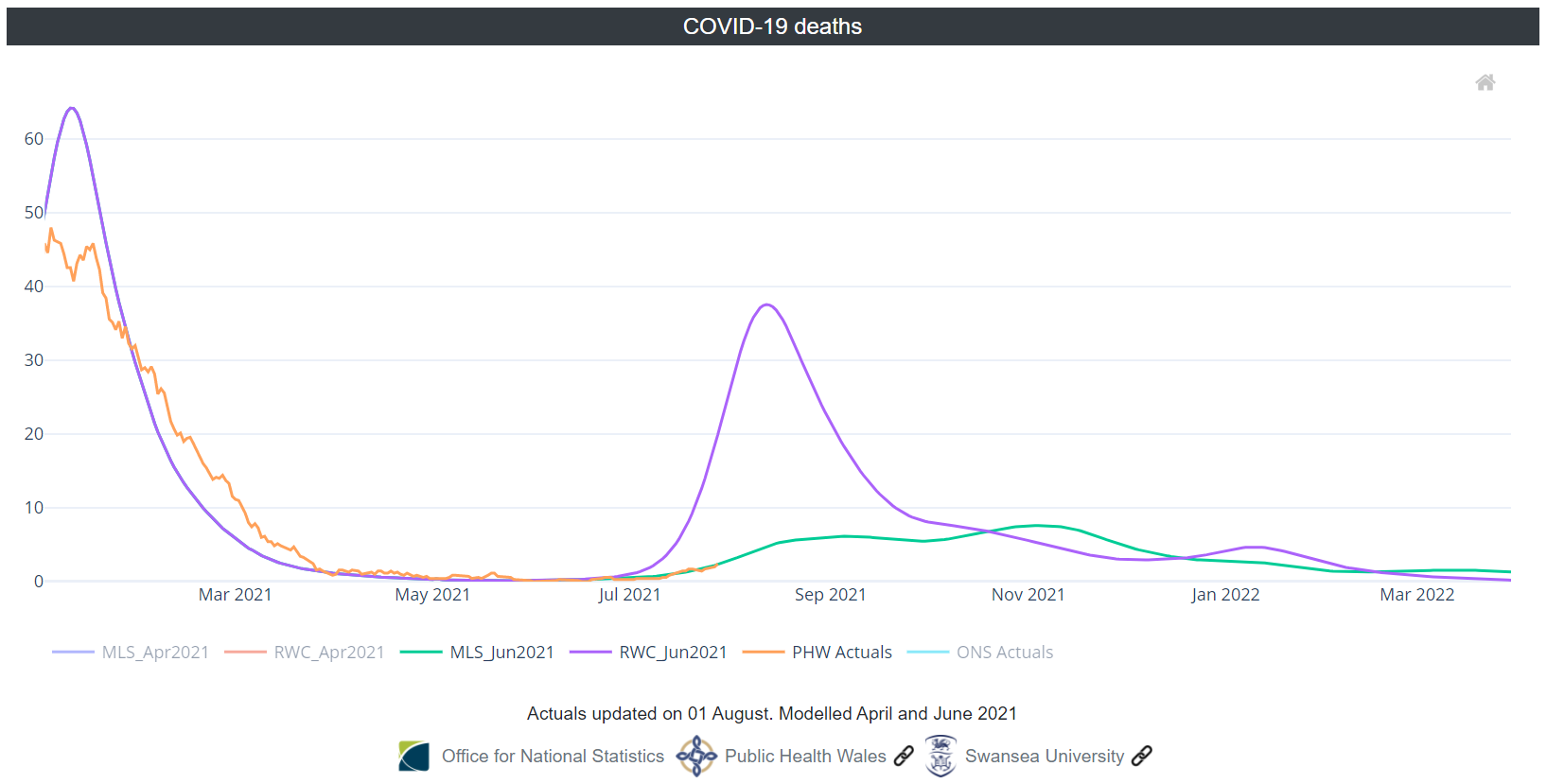
COVID-19 deaths were very low between April and mid-July 2021. They started to rise in mid-July and have followed the MLS closely since then.
Evidence outline: ventilation
Ventilation is an important COVID-19 mitigation measure and can reduce airborne transmission of SARS-CoV-2 beyond 2m, although it is unlikely to have significant impacts on close range transmission by droplets and aerosols (within 1-2m) or transmission via contact with surfaces (high confidence).
Priority should be given to improving ventilation of spaces which are most likely to result in a high transmission rate, such as multi-occupant spaces with very low ventilation rates and long duration of exposure (high confidence).
Ventilation should be considered alongside other control measures and the use of face coverings in certain settings is recommended. Face coverings will have greatest benefits where people are in close proximity or are in the same shared space for a period of time, especially where ventilation is poor or there is activity that could produce enhanced aerosols.
The effectiveness of ventilation in many environments is strongly influenced by user behaviour. Clear messaging and guidelines will be needed to improve understanding on the reasons why good ventilation is important and how to effectively operate ventilation systems or achieve good natural ventilation.
Increasing ventilation rates may have other negative consequences including financial, energy use, noise, security and health and wellbeing impacts from thermal discomfort and exposure to pollutants.
Schools and HE/FE settings are heterogeneous, with differences in class sizes, rules, structures, environmental conditions and ventilation rates. Ventilation is important in all school settings and will influence the potential for transmission in schools.
Indoor environments should be optimised to limit transmission of the virus and outdoor environments adapted for better use in winter. Ventilation is a key mitigation, particularly as people are less likely to open their windows and doors during winter.
The level of Carbon Dioxide (CO2) in a space can be used as a proxy for occupancy and ventilation, particularly in multi-occupant spaces (high confidence), though is not a direct proxy for infection risk and is less effective in low occupancy or large volume spaces (high confidence). CO2 monitoring can be a cost-effective way to identify spaces with high occupancy and/or poor ventilation to indicate where transmission events may be more likely to occur. However, compared to other mitigation measures (such as hand hygiene and cleaning surfaces), it is less well understood by individuals or organisations (medium confidence). This may be, in part, because it is less visible. CO2 monitoring may help make ventilation issues more observable and guide actions to manage ventilation either in the short term (such as opening windows) or longer-term (such as changes to systems).
The application of air cleaning devices may be useful to reduce airborne transmission risks in poorly ventilated spaces. Air cleaning devices are not a substitute for ventilation and should never be used as a reason to reduce ventilation. Ventilation should be assessed, and improved if possible, before considering using an air cleaner. Benefits of such devices diminish when ventilation increases unless there are specific risks identified.
Examples of improving ventilation to reduce transmission have been published by the Health and Safety Executive. The examples listed include improvements to portacabins and changing rooms, canteens and offices and production halls or packing rooms.
The UKRI funded ‘Adapting Offices’ project also emphasises the importance of good ventilation as people return to their place of work. Read their Stage 1 report.
The Royal Academy of Engineering has published its report ‘Infection Resilient Environments’, outlining a number of recommendations for Government.
Previously published TAG and SAGE papers for more information and a link to the relevant Welsh Government pages are available below:
- Taking reasonable measures to minimise the risk of exposure to coronavirus in workplaces and premises open to the public
- EMG: Role of ventilation in controlling SARS-CoV-2 transmission, 30 September 2020 - GOV.UK (www.gov.uk)
- EMG and SPI-B: Application of CO2 monitoring as an approach to managing ventilation to mitigate SARS-CoV-2 transmission, 27 May 2021 - GOV.UK
- Safe-schools-v4b1.pdf (independentsage.org)
- Healthier schools during the COVID-19 pandemic: ventilation, testing and vaccination (imperial.ac.uk)
- EMG and SPI-B: Application of CO2 monitoring as an approach to managing ventilation to mitigate SARS-CoV-2 transmission, 27 May 2021 - GOV.UK
- Technical Advisory Group: air cleaning devices, January 2021
COVID-19 evidence: round-up
Do members of the public think they should use lateral flow tests or PCR tests when they have COVID-19-like symptoms? The COVID-19 Rapid Survey of Adherence to Interventions and Responses [CORSAIR] study
This study aims to investigate public use of lateral flow test [LFT] or polymerase chain reaction [PCR] test when experiencing key COVID-19 symptoms through two waves of a nationally representative online survey of 3,665 adults living in England or Scotland. While the study does not consider a Welsh population, it does support the need for clear communication to the public around use of COVID-19 tests.
10% of respondents thought Government guidance stated that they should take an LFT if symptomatic, while 18% of people thought that should take a PCR test; 60% thought they should take both types of test (12% did not select either option). In people who were symptomatic, 32% reported taking a test to confirm whether they had COVID-19. Of these, 53% reported taking a PCR test and 44% reported taking an LFT.
Despite Government guidance stating that anyone with key COVID-19 symptoms should complete a PCR test, a significant percentage of the population use LFT tests when symptomatic, attributed to the easy accessibility of LFTs, short turnaround time and lack of requirement to formally register the test with the Government (and subsequently self-isolate on a positive test). Communications should emphasise the superiority of, and need for, PCR tests in people with symptoms.
Modelling rates of SARS-CoV-2 transmission during vaccination and likelihood of vaccine-resistant strains
A peer-reviewed mathematical modelling study has been published in Nature looking at the conditions that may increase the risk of the emergence and establishment of a vaccine-resistant variant of COVID-19.
The paper concludes that as a general principle policymakers and individuals should consider maintaining non-pharmaceutical interventions and transmission-reducing behaviours throughout the entire vaccination period.
…we found that a fast rate of vaccination decreases the probability of emergence of a resistant strain. Counterintuitively, when a relaxation of non-pharmaceutical interventions happened at a time when most individuals of the population have already been vaccinated the probability of emergence of a resistant strain was greatly increased. Consequently, we show that a period of transmission reduction close to the end of the vaccination campaign can substantially reduce the probability of resistant strain establishment.
The modelling suggests that this risk is highest when a large fraction of the population has been vaccinated alongside high rates of transmission, a situation that has recently been observed across much of the UK. As a result, ongoing public health surveillance and rapid sequencing of cases will be crucial to track the epidemiology of the pandemic and emergence of potential variants of concern.
The paper also emphasises the importance of supporting global vaccination efforts to reduce the chance of a global spread of a vaccine-resistant variant.
Link to paper: Rates of SARS-CoV-2 transmission and vaccination impact the fate of vaccine-resistant strains | Scientific Reports (nature.com)
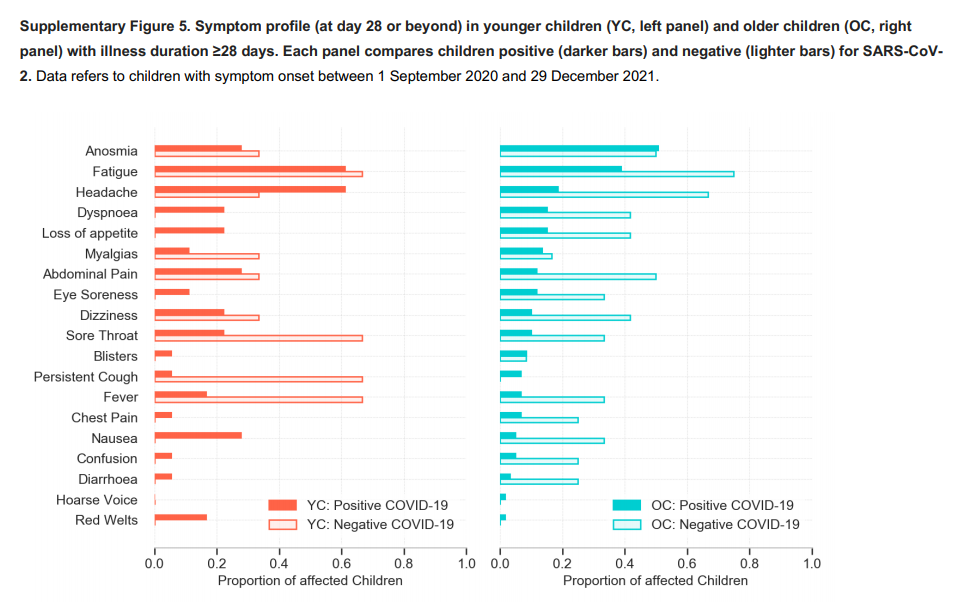
Study looking at long-lasting symptoms from COVID-19 in school-aged children: Zoe Tracker app
The results suggest that children aged 5-17 years infected with symptomatic SARS-CoV-2 infection are usually of short duration (6 days compared with 11 days in adults) with a low symptom burden. Children are also less likely to suffer prolonged symptoms after acute COVID-19 infection and the majority of those with persistent symptoms recover 2 months after illness (4.4% retain symptoms after 28 days and 1.8% after 56 days).
The most common symptoms in children were headache (62.2%) and fatigue (55.0%), compared to a meta-analysis of other studies that identified fever and cough as the most common symptoms (37.7% and 25.5% in this study’s analysis).
Whilst children with negative test results were less likely to suffer from prolonged symptoms (0.9% at 28 days), this cohort had a higher symptom burden than those testing positive for SARS-CoV-2.
It is important to note that this data is reported by parents and depended upon an adult with access and capacity to participate.
Long COVID, a comprehensive systematic scoping review
The controversies in its definition have impaired proper recognition and management. The predominant symptoms were: fatigue, breathlessness, arthralgia, sleep difficulties, and chest pain. Recent reports also point to the risk of long-term sequela with cutaneous, respiratory, cardiovascular, musculoskeletal, mental health, neurologic, and renal involvement in those who survive the acute phase of the illness.... This lack of well-defined criteria to define Long COVID-19 emphasizes the need for international-health-organizations, such as WHO, to address this issue.
Defining the factors that predict the development of Long COVID require more cohort and longitudinal studies. Since it is anticipated that there will be an enormous number of long COVID patients in the near future, identifying such predictors could help the Long COVID-specified clinics to prioritize the most vulnerable people and provide care to those in need.
Full paper: Long COVID, a comprehensive systematic scoping review | SpringerLink
Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine-breakthrough infections: a multi-center cohort study (pre-print)
This pre-print aims to study if vaccination alters virological and serological kinetics in breakthrough infections of SARS-Cov-2, using a multi-centre retrospective cohort study of patients in Singapore who had been admitted to hospital infected with the Delta variant, comparing clinical courses between fully vaccinated (with a licensed mRNA vaccine) and unvaccinated individuals.
It concludes that the mRNA vaccines are highly effective at preventing symptomatic and severe COVID-19 associated with B.1.617.2 infection. Vaccination is associated with faster decline in viral RNA load and a robust serological response. Vaccination remains a key strategy for control of COVID-19 pandemic.
Of 218 individuals with Delta variant infection, 84 had received a mRNA vaccine (of which 71 were fully vaccinated), 130 were unvaccinated and 4 received a non-mRNA vaccine. Despite significantly older age in the vaccine breakthrough group, the odds of severe COVID-19 requiring oxygen supplementation was significantly lower following vaccination (adjusted odds ratio 0.07 95%CI: 0.015-0.335). PCR cycle threshold (Ct) values were similar between both vaccinated and unvaccinated groups at diagnosis, but viral loads decreased faster in vaccinated individuals. Early, robust boosting of anti-spike protein antibodies was observed in vaccinated patients, however, these titers were significantly lower against Delta as compared with the wildtype vaccine strain.”
Social contacts in the UK from the CoMix social contact survey: week 70
Mean reported contacts [in the UK] do not appear to have increased since the easing of restrictions on July 19th. Overall, contacts amongst adults remain stable, whereas contacts for children have decreased sharply now that schools have closed.
Reported contact rates for children are similar to that observed last summer and are much lower than during periods when schools are open.
Reported contact rates for younger adults appear to be lower than was reported last summer though the number of participants in this age group have been smaller for the prior two weeks of data. Older adults are reporting roughly similar levels of contact as during summer of 2020.
The proportion of participating children isolating has sharply decreased, but remains in excess of 10% and remains more than twice as high as the proportion of adults who are self-isolating.
There may be an early indication that levels of mask-wearing may have fallen slightly. However, overall rates of mask wearing remain high.
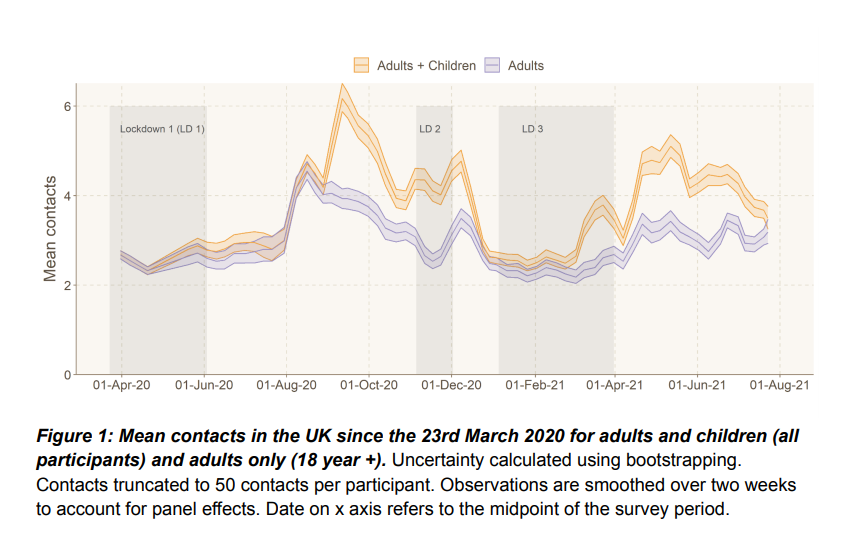
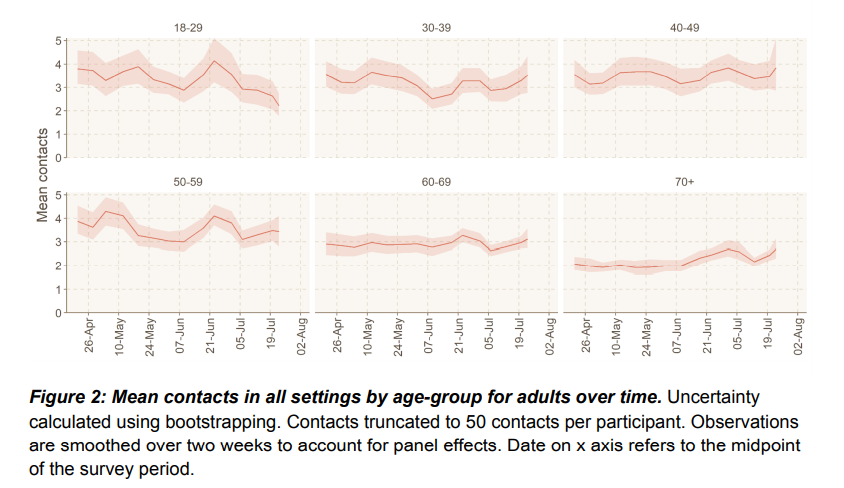
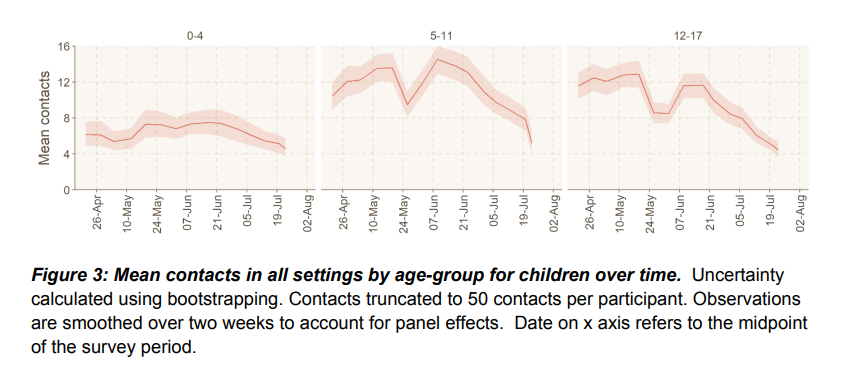
Full paper: Comix Report Survey Week 70 (cmmid.github.io)
Investigation into myocarditis associated with COVID-19 mRNA vaccination – United States
Last month the CDC published a paper supporting its recommendations for the use of the Pfizer and Moderna COVID-19 mRNA vaccines in children age 12 and above, follow reports of myocarditis and pericarditis in this group.
Myocarditis is an inflammation of the heart muscle responsible for contracting and relaxing to pump blood in and out of the heart and to the rest of the body. Symptoms typically include abnormal heartbeat, chest pain, or trouble breathing. Pericarditis is an inflammation of the thin tissue surrounding the heart (the pericardium) resulting in chest pain and a high temperature. Most cases are mild and temporary.
After reports of myocarditis and pericarditis in mRNA vaccine recipients, which predominantly occurred in young males after the second dose, the US Advisory Committee on Immunization Practices (ACIP) reviewed the cases of myocarditis with regard to the benefit vs risk balance of mRNA COVID-19 vaccination.
Under the US Vaccine Adverse Event Reporting System, 687 cases of myocarditis in people aged under 30 after mRNA vaccination were reported during the period 29 December 2020 to 11 June 2021, out of a total of 30 million first doses and 22 million second doses of mRNA vaccines administered to that age group.
The ACIP concluded that the benefits of mRNA COVID-19 outweighs the risks, including in adolescents and young adults, although there was recognition the balance of benefits and risks varied by age and sex. Outcomes of myocarditis cases will continue to be monitored and it was recommended that providers and the public should be informed about these cases to inform their own risk assessment, particularly for males aged 12-29 years.
Public attitudes towards COVID-19 vaccination in children: a qualitative study
Focus groups and interviews revealed how COVID-19 vaccination in children was framed as a complex problem (a “minefield”).
Six themes emerged to explain participants views: (1) Uncertainty over whether children can catch, transmit or be severely harmed by COVID-19; (2) Lower risk tolerance for unknown longer-term effects of the vaccine in children; (3) Association of the vaccine program with government’s handling of the pandemic; (4) Local social norms as a driver of hesitancy; (5) Vaccinating children as a way to protect vulnerable adults; (6) Children’s vaccination as parental choice.
Public attitudes to COVID-19 vaccination in children are likely to be met with more hesitancy compared to adult vaccinations.
Linking to our previous research on attitudes towards adult vaccinations, it may be that a social norm around vaccination in children is yet to build (and might do so once the vaccine is approved for use in children in the UK, and in more countries globally)
The lower risk tolerance and lower perceived benefits, coupled with the fact many want to wait until more evidence is available, suggests that there is a high burden of proof regarding the vaccines safety for children, and that the cost-benefit ratio for some may not be perceived as currently high enough. Clear and official scientific communications once approved may aid uptake if and when relevant.
Public health communications will need to combat this hesitancy if vaccine uptake for children is to be pursued as a public health policy. Communication to parents (and the public): (1) the safety of the vaccine in children; (2) the benefits of the vaccine to the children themselves, and, if relevant, (3) the benefits of the vaccine in children to the overall reduction of transmission in the population overall (including the lowering of risk to vulnerable family/community members).
Full paper: Public attitudes towards COVID-19 vaccination in children: A qualitative study (medrxiv.org)
TAG: Moral Injury in Health Care Workers during the COVID-19 Pandemic
Moral injury can occur when someone engages in, fails to prevent, or witnesses acts that conflict with their values or beliefs and when they experience betrayal by trusted others especially when this is perceived as avoidable, or they are powerless to change it. Healthcare workers may be/ have been at increased risk of exposure to potentially morally injurious experiences (PMIEs) because of the COVID-19 pandemic.
Examples include: when present at a patient’s death without loved ones present; allocating restricted resources to severely unwell patients; and feeling let down by others with regards to their safety. Moral injury is not a mental illness but can contribute to other mental health problems, such as Post-Traumatic Stress Disorder (PTSD), stress, as well as low morale and hostility.
Long-term negative outcomes in healthcare workers of exposure to PMIEs and consequent impacts for patients and the organisations they work in are not inevitable. Health care workers, their colleagues, and leaders can use strategies to improve outcomes both during and after potential morally injurious situations, to support recovery. These include:
- Preparation for the likely moral injuries they will face
- Processes to support shared team decision making and responsibility
- Peer support mechanisms and programmes
- Staff reporting psychological distress should be identified early and offered specialist support. Consider active monitoring due to issues with help-seeking
- Where distress is longer term or associated with mental ill-health, such as PTSD, specialist support and evidence-based interventions should be available accordingly
Full paper: Technical Advisory Group: moral injury in health care workers during the COVID-19 pandemic.
Technical Advisory Group: COVID-19 population immunity estimates in Wales
Assuming immunity wanes after 2 years, 82% [64%, 85%] of people aged 16 and over in Wales were estimated to have had some immunity against COVID-19 infection at 24 July 2021.
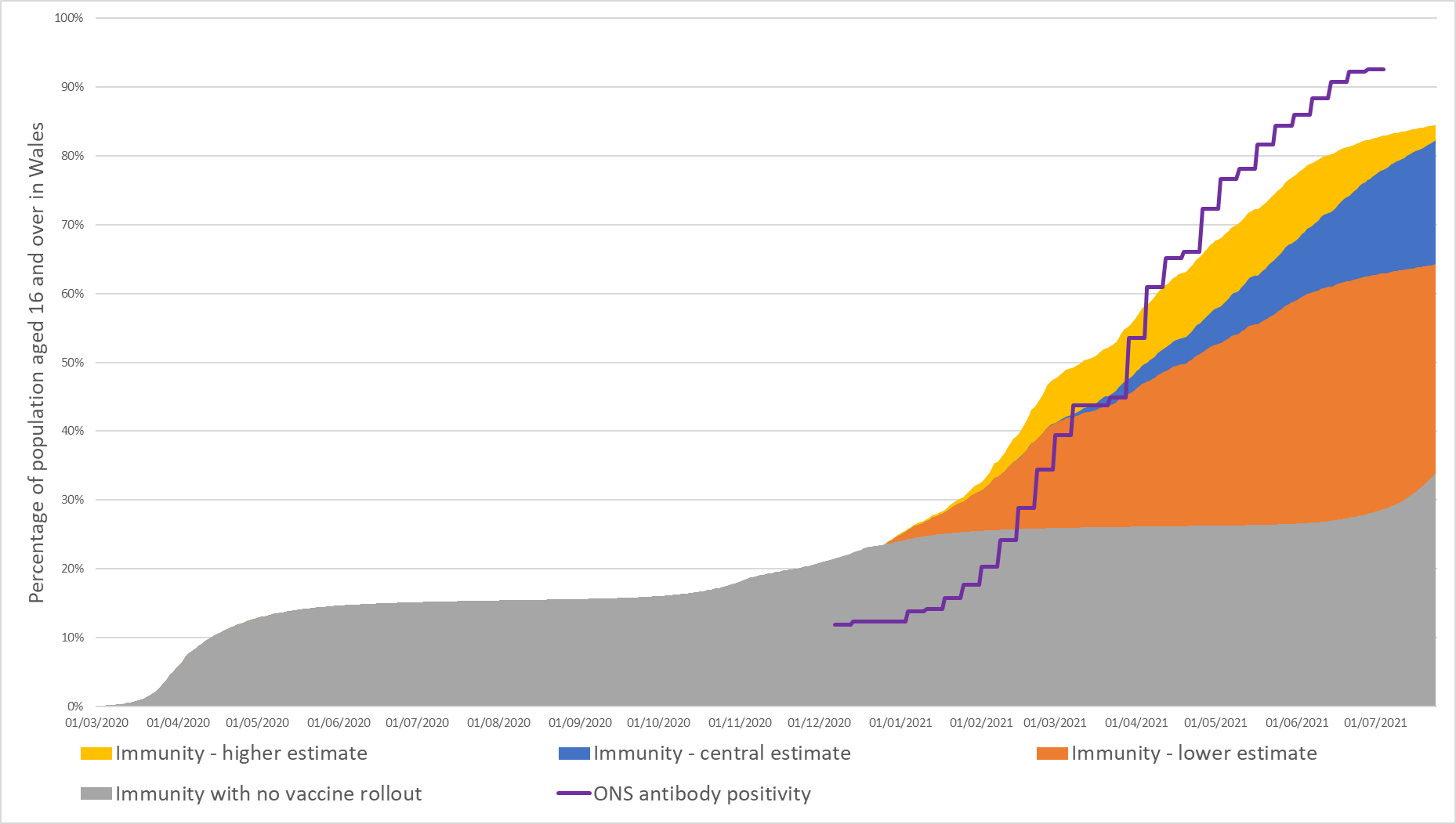
Immunity estimates and antibody status of individuals aged 16 and over in Wales, to 24 July 2021, assuming immunity wanes after 2 years.
Assuming immunity wanes after 2 years, 70% [56%, 72%] of the total population in Wales were estimated to have had some immunity against COVID-19 infection at 24 July 2021.
Immunity levels varied across age groups. Highest immunity was estimated in individuals aged 80 and over at 97% [70%, 97%] at 24 July 2021. Lowest immunity (excluding individuals aged under 16) was estimated in individuals aged 16 to 19 at 55% [53%, 61%] at 24 July 2021.
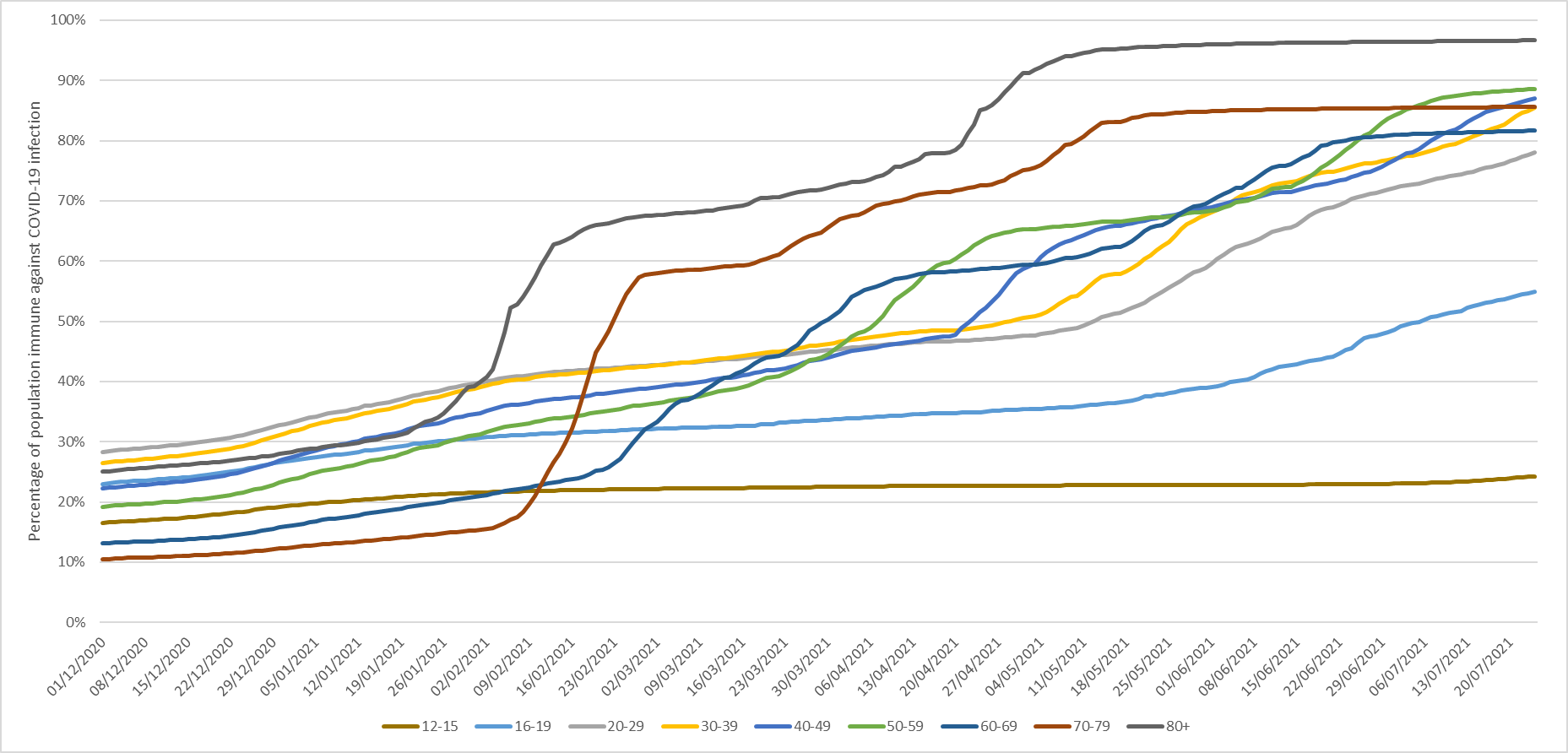
Immunity estimates in Wales, by age group, to 24 July 2021, assuming immunity wanes after 2 years.
Immunity levels in the population have been significantly increased by the vaccine rollout. If no vaccines had been administered, it was estimated that 34% of people aged 16 and over in Wales (32% of the total population) would have had some immunity against COVID-19 infection at 24 July 2021.
It is estimated that over 80% (may be closer to 90%) of the Welsh population, spread evenly across Wales, must be immune to COVID-19 before population immunity effects could be observed. As a result there is still a way to go before population immunity effects could be observed.
Full paper: Technical Advisory Group: COVID-19 population immunity estimates in Wales.
